What the news & your obesity doctor won’t tell you about Ozempic and Mounjaro.
Many of my patients have come to me with questions about this new class of medications that are being used for both diabetes and weight loss. The new blockbusters are called Ozempic and Mounjaro and seemingly every celebrity has tried it. Some with wild success and others have seemingly already gained the weight back. The question everyone should be asking is what are the benefits and what are the risks?

Firstly, the results on weight loss are actually quite impressive and the duration of the studies are fairly long-term for diabetes and weight loss. In this two years study, it’s clear that the drug helped produce a 15% weight loss that seemed to sustain through to 2 years. The drug also causes fewer heart attacks than a placebo which is reassuring compared to prior debacles with weight loss medications like Phen-Fen that were implicated in heart pathology and eventually removed from the market.
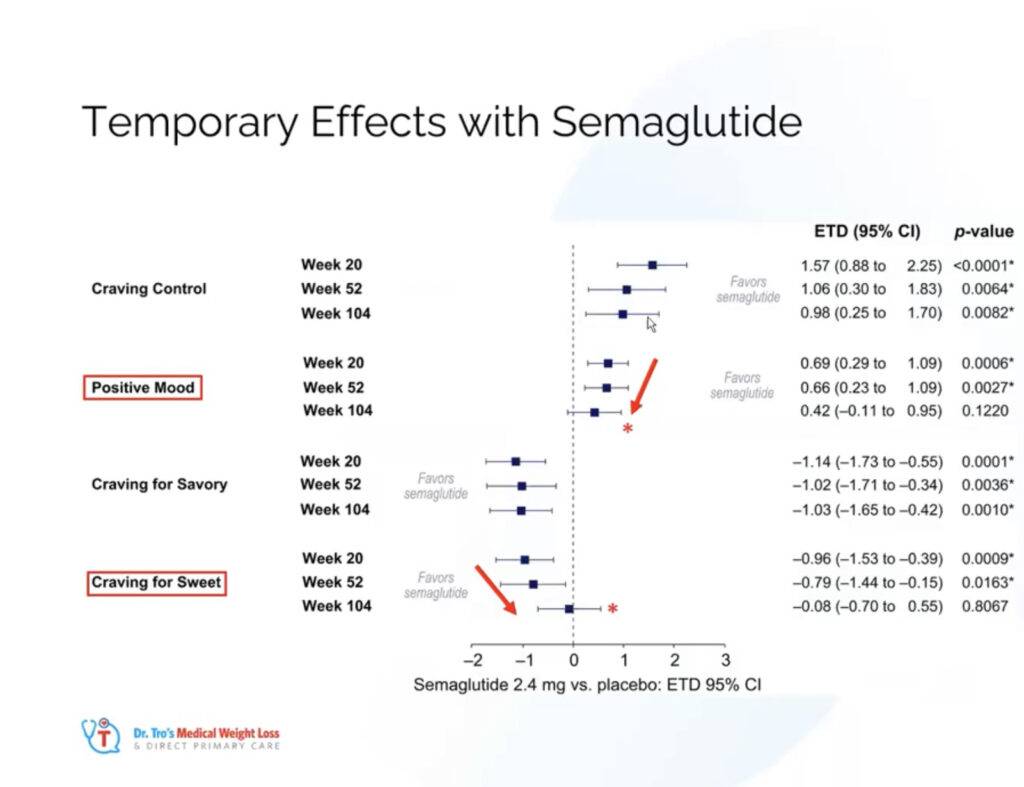
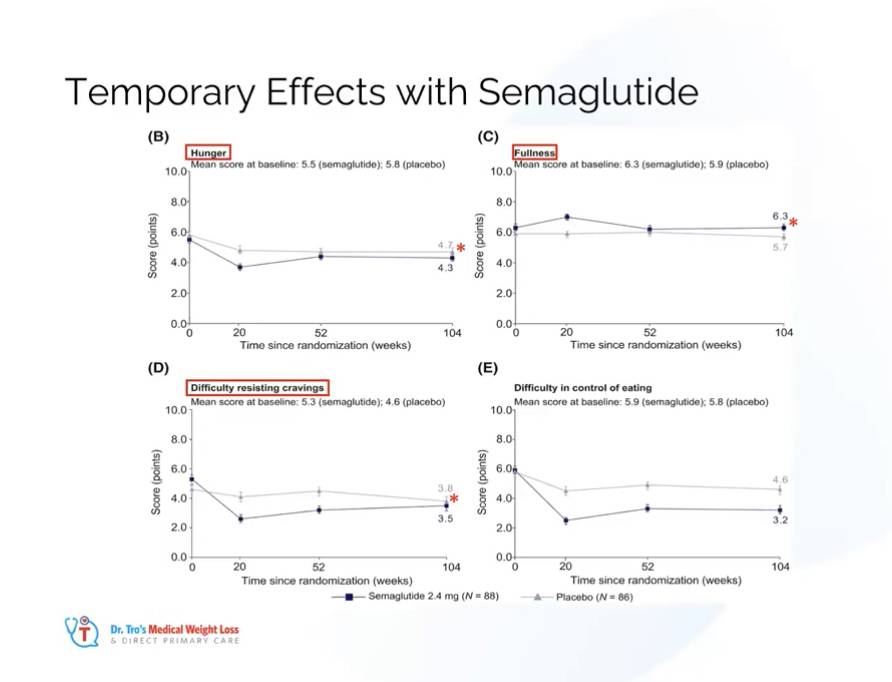
But I want all my patients and the public to know that the appetite and weight loss effects do not last forever. Effects on hunger, cravings control, sweet cravings, mood & fullness are TEMPORARY and return to baseline between years 1 & 2. This was shown in surveys taken from patients using the medication over the long term.
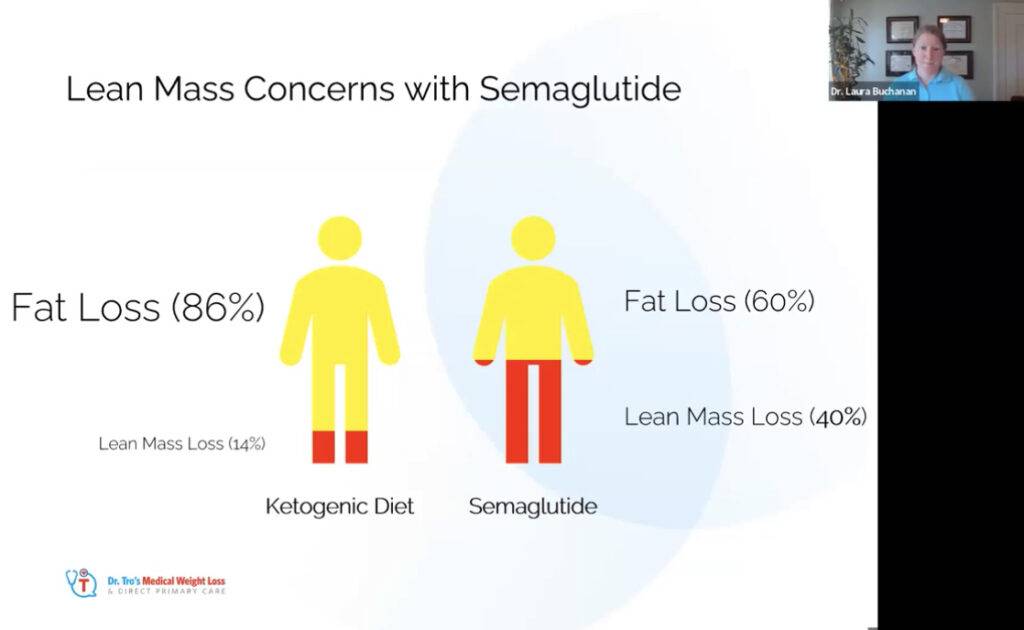
Furthermore, if the treatment isn’t coupled with aggressive resistance training and high protein intake, there can be up to 40% lean mass loss, which is in stark contrast to the data we have reviewed for low-carb and ketogenic diets.
I want to clarify that while the drug undeniably provides weight loss and diabetes benefits, it is important to be aware of both its capabilities and limitations.
It is crucial to recognize that the drug in question serves as a temporary aid or a crutch, rather than a permanent solution. Many approaches to managing obesity often turn out to be ineffective or temporary solutions, akin to failed crutches.
Take lap bands as your omen.
After 1,000,000 lap bands placed worldwide by obesity doctors, the most common lap band surgery TODAY is lap band removal.
Pharma & your doctors don’t care about lasting changes, their history and track record are clear. The industry is experiencing RECORD PROFITS, yet our population has more diabetes and obesity than EVER.
To achieve lasting health and well-being, it is advisable to seek out a medical team that genuinely cares about your journey. Consider joining a community of individuals who are actively addressing obesity, regardless of whether they have undergone surgery, use medication, or have chosen not to pursue those options—like myself. Find a team that is committed to supporting your long-term vision of health, rather than one that promotes quick fixes or temporary solutions as ultimate cures, of which there are many.
Many telehealth companies are aggressively marketing these drugs in quick online visits, and while providing access to care is noble, where will they be when their patients fail?
If you are taking Ozempic or Mounjaro, it is important to consider incorporating certain practices into your routine.
- A high-protein diet can be beneficial.
- Including ample protein in meals can help promote satiety, preserve muscle mass, and support overall weight management efforts. Since your total volume of eating will be less, aim for approximately 1 gram of protein per pound of your ideal body weight, and distribute it across 2-3 meals throughout the day.
- Integrating regular resistance training into your fitness regimen is highly recommended.
- In resistance exercises, such as weightlifting or bodyweight exercises, 4-6 times per week can help build and maintain muscle mass. Make sure you are doing resistance training nearly daily. Aim to target each major muscle group at least twice per week, incorporating high-volume workouts
Many patients have successfully stopped these medications in our practice without weight regain and these two factors have been critical to safely stopping this medication in our practice.
Our approach is to use the drug for the shortest necessary period to achieve the desired outcome or therapeutic effect and taper the drug gradually, typically lowering the dose every 4 weeks. We have achieved significant success in discontinuing this medication without experiencing weight regain and, in many cases, even witnessing further weight loss.
My true contention isn’t with these GLP1 drugs, it’s physicians being responsible. Expecting our patients to implement lifestyle changes in 7-minute visits is insane and do we really expect doctors to responsibly counsel somebody through GLP1 usage? Doctors have used glp1 in weight loss for 5+years and 10+ years for diabetes. Every week, seemingly we have new & countless consults for people who have failed or regained weight on these medications. I am not saying this will be true for all but the tide is turning and I expect a tsunami of weight regain after 1-2 years of use similar to every other weight loss intervention. These consults are so common for us that it is now normal and expected.
My issue isn’t with the drugs per se but I am concerned about my profession and our lack of commitment to people who need help. Instead corporate doctors pawn off $100/month scripts with little-to-no support and more blaming the victim when the drug stops working. We need to do better.
If you are seeking additional resources on metabolic health or a self-guided medical weight loss curriculum, I recommend exploring our app, which provides comprehensive support for starting your journey at your own pace. Alongside connecting with a vibrant community, our team is dedicated to offering guidance and assistance whenever you need it. Feel free to take advantage of these resources to enhance your progress and achieve your goals.






